Byram_Patrik
New Member
- 2
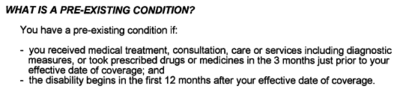
I have a group policy. I was on short-term disability first and was unable to return to work after the 12 weeks were up, so my claim turned into a long-term claim. For long-term it was initially approved but then they came back under reservation of rights a few months later and denied it, citing pre-existing conditions. I didn't think that the pre-existing conditions clause applied, however, because the date of my long-term claim was post the 1-year policy holding period requirement. But they said that they could use the date of my short-term claim as the date of my disability, which was within the 1-year period (complex, I know...) Anyway, my question is: can they do this? How could they know that my short-term application date was definitively my disability date? Said another way, how could they know that I wasn't disabled long-term until the "transition date" from short-term to long-term? It seems to me that they can't, and they are only claiming this in order to cite the pre-existing condition clause and deny my claim.
I have an attorney who says appeal could go either way (gee, thanks for the expert insight), says policy language is ambiguous. Recommends going back to work for a period of time to negate the ambiguity altogether but that's FAR easier said than done. Further, I fear I'll be termed if I return to work, in which case I'll have no policy whatsoever. So, I'm learning towards appeal but want to know how much I should stress this point relative to other salient points.
Help?
I greatly appreciate any help anyone can provide - it really means a lot to me.
I have an attorney who says appeal could go either way (gee, thanks for the expert insight), says policy language is ambiguous. Recommends going back to work for a period of time to negate the ambiguity altogether but that's FAR easier said than done. Further, I fear I'll be termed if I return to work, in which case I'll have no policy whatsoever. So, I'm learning towards appeal but want to know how much I should stress this point relative to other salient points.
Help?
I greatly appreciate any help anyone can provide - it really means a lot to me.