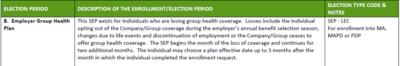
Coming off employer coverage...
You get an 8-month SEP for enrolling in Medicare.
You get the 6-month OEP for MedSupp , that starts When Part B starts.
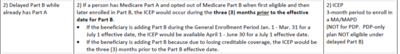
For MAPD... during the ICEP, you only get 3 months that take place before Part B begins, which is odd.
So... someone would have to sign up for MAPD first, then Medicare?
What are the specifics of how that works?
You get an 8-month SEP for enrolling in Medicare.
You get the 6-month OEP for MedSupp , that starts When Part B starts.
For MAPD... during the ICEP, you only get 3 months that take place before Part B begins, which is odd.
So... someone would have to sign up for MAPD first, then Medicare?
What are the specifics of how that works?