sk337sk337
Expert
- 54
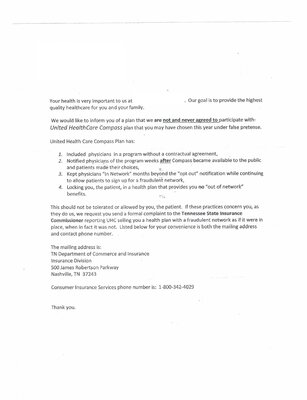
I was just emailed the attached image from an insured. I took some of their personal information out. I've had a few clients tell me their doctors were listed as in-network but now are being told they are not accepting this plan or something similar to the letter. Most of the people who are telling me about the issues are on exchange but no subsidy. We chose these plans BECAUSE they were their best option on/off exchange. (In East TN we only have two options: UHC or BCBS) How would you handle this? Is anyone else having this happen?