I had eyelid surgery which consisted Ptosis repair (rising up upper muscle) Blepharoplasty (removal of extra skin that is holding over my eyes). They are usually done together as it’s the same incision. Both were to fix impaired vision due to my eyelids obstructing my field of vision. Surgeon sent PA for both procedures and both were approved.
When surgery was scheduled I was told that only Ptosis repair would be performed and Blepharoplasty would be done at another time because insurance would only cover one at a time. I called insurance and spoke to a manager, and she said that both procedures will be covered if done together as they are both in the prior authorization. So she called the doctors office and explained and the doctors office agreed to schedule the surgery for both procedures at the same time. However, they did make me sign a document saying that both procedures may not be covered, and I would be responsible for the balance, if they are not covered.
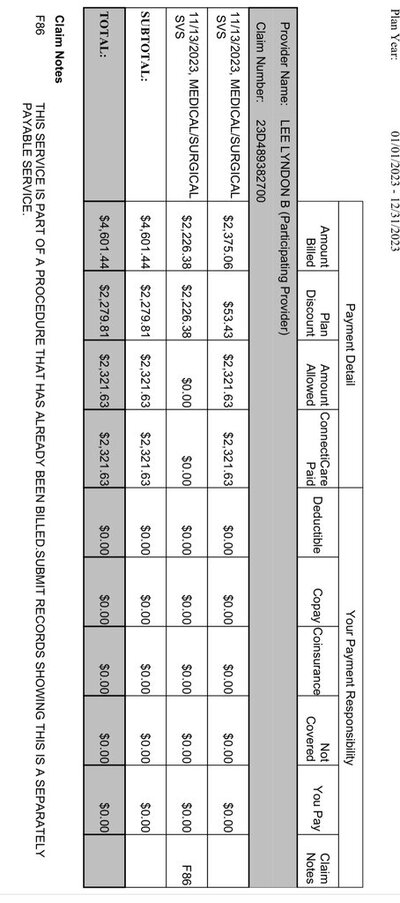
Now, to my surprise, only the ptosis repair was covered, and the other was bundled into the procedure as they are mutually exclusive. So technically the insurance paid for both procedures as part of one procedure. And the doctor’s office wants me to pay the difference (over 2k). The explanation of benefits says that I have zero responsibility.
On one side, the doctors office tells me that they made me aware that it will not be covered and I signed the document saying that I will pay for it. And on the other side, I have the insurance saying that they did pay for both procedures as both procedures codes are in the payment, but they say that if I signed a document that is between the Doctor and I.
What should I do in this situation? Can I argue that the procedure was technically paid for? Does the insurance have any obligation to prohibit them from charging me when I have 0 responsibility?
When surgery was scheduled I was told that only Ptosis repair would be performed and Blepharoplasty would be done at another time because insurance would only cover one at a time. I called insurance and spoke to a manager, and she said that both procedures will be covered if done together as they are both in the prior authorization. So she called the doctors office and explained and the doctors office agreed to schedule the surgery for both procedures at the same time. However, they did make me sign a document saying that both procedures may not be covered, and I would be responsible for the balance, if they are not covered.
Now, to my surprise, only the ptosis repair was covered, and the other was bundled into the procedure as they are mutually exclusive. So technically the insurance paid for both procedures as part of one procedure. And the doctor’s office wants me to pay the difference (over 2k). The explanation of benefits says that I have zero responsibility.
On one side, the doctors office tells me that they made me aware that it will not be covered and I signed the document saying that I will pay for it. And on the other side, I have the insurance saying that they did pay for both procedures as both procedures codes are in the payment, but they say that if I signed a document that is between the Doctor and I.
What should I do in this situation? Can I argue that the procedure was technically paid for? Does the insurance have any obligation to prohibit them from charging me when I have 0 responsibility?