Truce
Expert
- 96
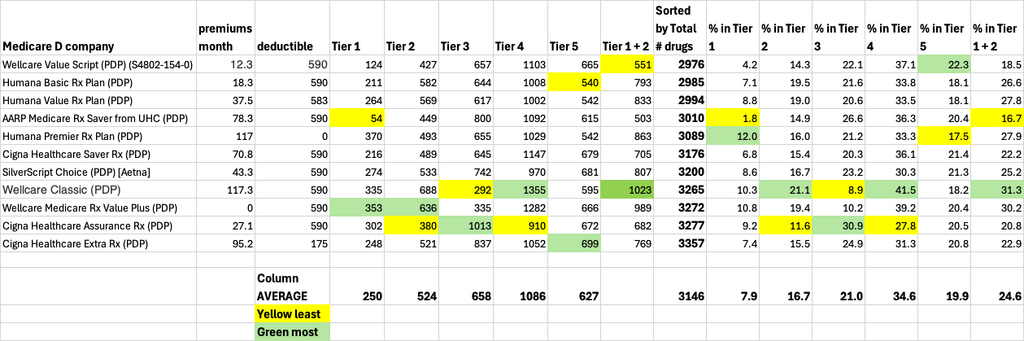
Wellcare has taken a few meds that were tier 3 last year and switched to a tier 2. Here's two I did today where members were using Goodrx/Cost Plus and now can just fill using their Value Script when auto renewing. No, you will not be paid for sharing this information with your clients.
Ezetimibe
risedronate sodium
Ezetimibe
risedronate sodium