Packerland
Guru
- 509
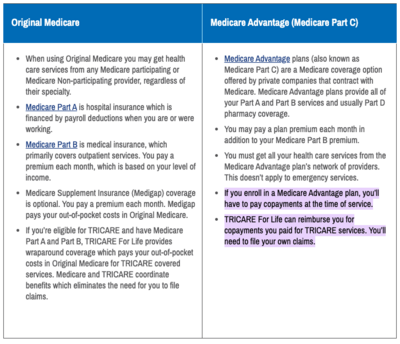
I have seen a couple of discussions regarding Tri-Care.
I hope this clears it up for some of you.
https://www.tricare.mil/Plans/HealthPlans/TFL/TFL_OHI
I hope this clears it up for some of you.
https://www.tricare.mil/Plans/HealthPlans/TFL/TFL_OHI